Abstract
Introduction: Ibrutinib, an oral Bruton Kinase inhibitor, is a highly effective treatment for patients with chronic lymphocytic leukemia (CLL). Previous studies reported an increased risk of bleeding due to impaired platelet function. Patients with CLL experience significant thrombocytopenia, which increases their risk for bleeding. This population was excluded from major trials and data is lacking to inform management in this setting.
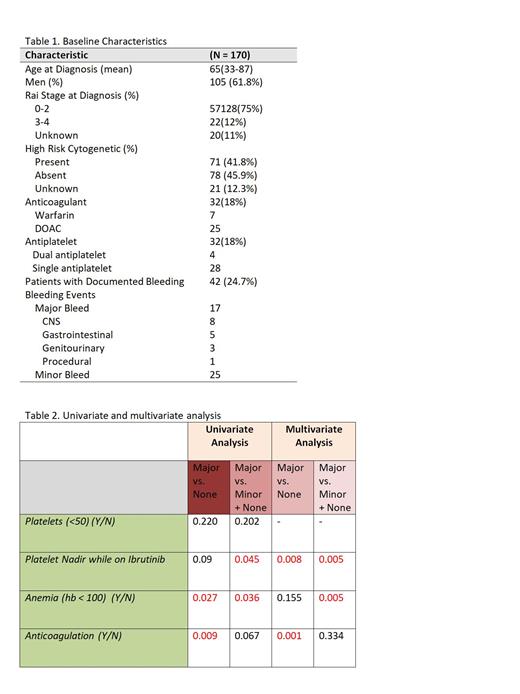
Methods: This is a single center retrospective study of all adult patients with CLL who received single agent ibrutinib in London, Ontario, Canada between January 2014 to December 2020. The primary objective was to investigate the risk of major bleeding associated with thrombocytopenia. Secondary objective was to investigate potential predictors of bleeding. Bleeding events were graded according to the National Cancer Institute Common Terminology Criteria for Adverse Events (CTCAE) grading system. A major bleed was defined as CTCAE grade 3 or higher as well as bleeding in the central nervous system. To assess the effect of independent variables on the outcome of bleeding, univariate analysis using chi square and t-tests was performed. Multivariate analysis was then preformed with the variables that were significant (p<0.05) on univariate analysis, using logistic and cox regression models.
Results: A total of 170 patients were included in this study. There were 54 bleeding events documented in 42 patients (24.7 %) of which 19(35 %) were major bleeding occurring in 17 patients. Median time to major bleeding was 2.4 months. Of the patients with major bleeding, 4(21%) were on anticoagulation, 2(10%) were on antiplatelet and 2(10%) were on combined anticoagulation and antiplatelet. There were 8 central nervous system (CNS) bleeding and 2 of them died. The mean platelet (PLT) nadir, defined as lowest PLT count at any point during ibrutinib treatment, was 73 x 10 9/Lin patients with major bleeding compared to 116 x 10 9/L in patients with minor and 91 x 10 9/L in patients with no bleeding events.
On the univariate analysis, when compared patients with major bleeding to patients with no bleeding, potential predictors of major bleeding included PLT nadir (p=0.09), haemoglobin (Hb) < 100 g/L at ibrutinib initiation (p=0.027) and anticoagulation (p=0.009). When compared patients with major bleeding to patients with minor or no bleeding, potential predictors of major bleeding included PLT nadir (p=0.045), Hb <100 (p=0.036) and anticoagulation (p=0.06). Grade 3 thrombocytopenia, defined as PLT nadir < 50 at any point during treatment with ibrutinib was not associated with increased risk of major bleeding (p=0.2).
To confirm the significance of these variables, multivariate analysis was performed. When compared patients with major bleeding to patients with no bleeding, PLT nadir (OR= 0.9, p=0.008) and anticoagulation (OR=4.02, p=0.001) were confirmed to be the potential predictors of major bleeding. When compared patients with major bleeding to patients with minor or no bleeding, PLT nadir (OR=0.9 p=0.005) and Hb <100 (OR=2.34, p=0.005) were the potential predictors of major bleeding.
Conclusions: Although not common, Ibrutinib is associated with increased risk of bleeding and identifying high risk patients is essential to prevent major bleeding events. This retrospective Canadian study was done with the primary objective to assess the association between PLT count and major bleeding in patients on ibrutinib for treatment of CLL. In this analysis patients with major bleeding tend to have lower PLT counts compared to patients with minor or no bleeding, with mean PLT nadir of 73x 10 9/L. However, grade 3 thrombocytopenia (PLT nadir<50) was not associated with increased risk of major bleeding. Other important predictors of increased risk of major bleeding while on ibrutinib include anticoagulation and anemia (Hb <100).
Louzada: Amgen: Honoraria; Pfizer: Honoraria; Celgene: Honoraria; Janssen: Honoraria. Lam: AbbVie: Honoraria, Membership on an entity's Board of Directors or advisory committees; Millennium: Honoraria, Membership on an entity's Board of Directors or advisory committees; Amgen: Honoraria, Membership on an entity's Board of Directors or advisory committees; Hoffmann-La Roche: Honoraria, Membership on an entity's Board of Directors or advisory committees; SeaGen: Honoraria, Membership on an entity's Board of Directors or advisory committees; Janssen: Honoraria, Membership on an entity's Board of Directors or advisory committees; Bristol-Meyers Squibb: Honoraria, Membership on an entity's Board of Directors or advisory committees; Servier: Honoraria, Membership on an entity's Board of Directors or advisory committees; Novartis: Honoraria, Membership on an entity's Board of Directors or advisory committees; Gilead: Honoraria, Membership on an entity's Board of Directors or advisory committees; Johnson & Johnson: Honoraria, Membership on an entity's Board of Directors or advisory committees; AstraZeneca: Honoraria, Membership on an entity's Board of Directors or advisory committees; Beigene: Honoraria, Membership on an entity's Board of Directors or advisory committees; Sanofi: Honoraria, Membership on an entity's Board of Directors or advisory committees; Pfizer: Honoraria, Membership on an entity's Board of Directors or advisory committees. Phua: Amgen: Honoraria; Janssen: Honoraria, Membership on an entity's Board of Directors or advisory committees; Takeda: Honoraria, Membership on an entity's Board of Directors or advisory committees; Pfizer: Honoraria; NovoNordisk: Honoraria, Membership on an entity's Board of Directors or advisory committees; AstraZeneca: Honoraria.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal